Post-vasectomy semen analysis (PVSA) is a crucial but often challenging step to confirm the success of a vasectomy procedure. Compliance with PVSA has been difficult due to various factors, including patient inconvenience, discomfort, time constraints, and the distance to a lab or clinic for testing. From a physician’s standpoint, following up with patients can require significant staff time to enable high compliance rates. In this blog post, we will review studies that examine the historical challenges associated with PVSA compliance and discuss the benefits of Fellow’s Vasectomy Test.
Poor Compliance With Postvasectomy Semen Testing: Analysis of Factors and Barriers, by Aaron Bradshaw et al.[1]: In this retrospective study assessing PVSA compliance over 12 years at the San Diego Veterans Administration Hospital and UC San Diego Health, among 503 patients that had a vasectomy, only 53% completed the recommended PVSA. Telephone interviews revealed that distance, time constraints, and forgetfulness were the primary barriers to completing the semen analysis. In addition, patients were asked if they were more likely to complete testing if the testing was home-based, and 92% responded yes.
Understanding the factors that influence compliance with post-vasectomy semen analysis, by Jon Duplisea et al.[2]: In a retrospective, single-institution study assessing 946 post-vasectomy patients, the authors identified several reasons for not obtaining PVSA including patients' misconceptions about achieving immediate sterility, discomfort during in person SA testing, and inconvenience due to multiple visits to provide a semen sample. The authors highlight the need for healthcare providers to address these barriers to improve compliance rates.
Post-vasectomy semen analysis compliance with use of a home-based test, by James Trussler et al.[3]: In a retrospective study of vasectomies performed by three providers, the authors compared the use of traditional office-based PVSA for 141 patients with the use of home-based PVSA testing for 85 patients. While the home-based group achieved a higher compliance rate (77%) relative to the office-based group (66%), this difference did not achieve statistical significance (p = .10). This study suggests that home-based testing can be part of the solution to solving the compliance challenge.
Scheduling Appointments for Postvasectomy Semen Analysis Has No Impact on Compliance, by Frederick Jacobsen et al.[4]: In a retrospective study of 400 vasectomy patients, the authors examined the impact of a policy change requiring appointments for semen sample drop off, rather than the previous policy of not requiring an appointment. For the 200 patients required to schedule an appointment, compliance rose (80%) compared to the earlier group without this requirement (74%); however, this difference did not reach statistical significance (p = 0.19).
Fellow Vasectomy Testing: A Solution to Poor Compliance
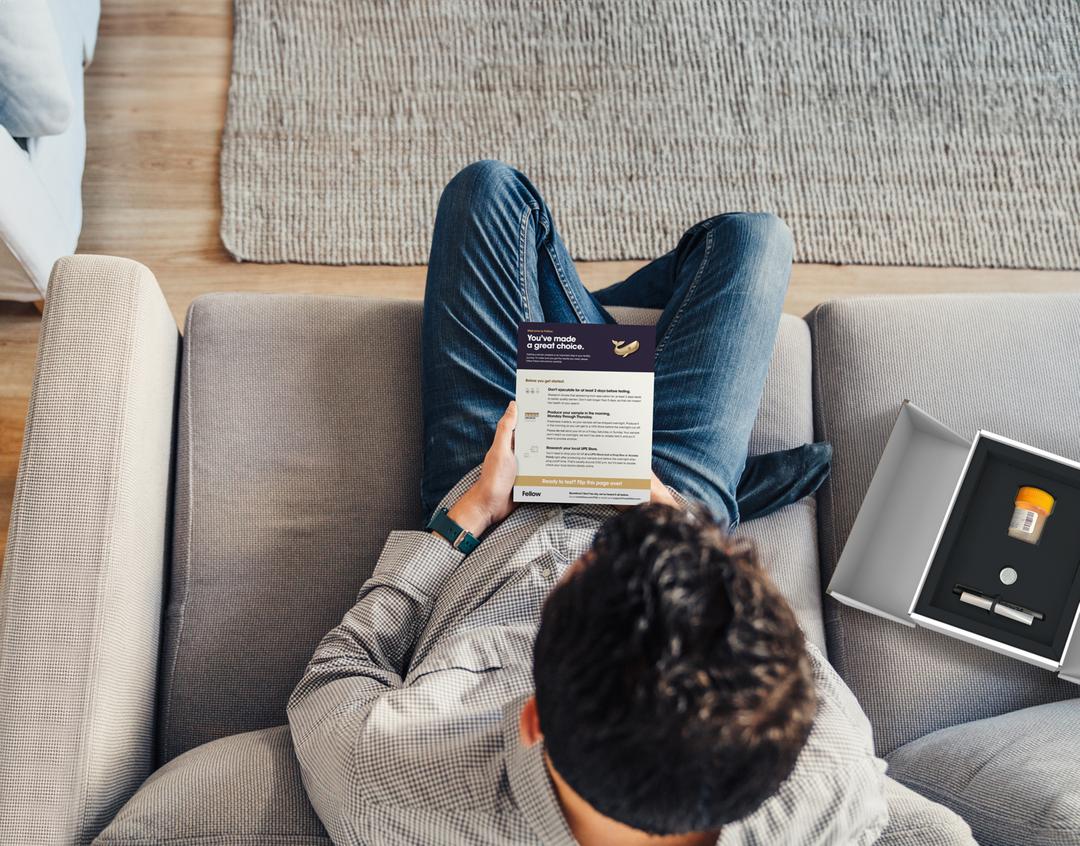
Our work at Fellow builds on this understanding of the challenges clinics face and their possible solutions. Fellow enables a new method to improve compliance using mail-in semen analysis working in tandem with a robust patient engagement system that encourages patients to complete testing. Mail-in testing offers a convenient and patient-friendly alternative to the traditional 1-hour semen analysis, allowing a patient to collect a semen sample in the privacy of their own home and send it to Fellow’s CLIA laboratory for analysis. The benefits of Fellow’s approach include:
Benefits for Clinics:
Automated Patient Follow-Up: Fellow reminds the patient to complete testing 12 weeks after their vasectomy, and will continue to follow up to complete testing. In addition, each patient’s test status can be tracked within the Fellow online portal.
Prompt Results Delivery and Automatic Re-Testing: Results are sent directly to both the patient and clinic in an easy-to-understand format. If ANY sperm cells are observed, Fellow automatically re-tests the patient at no-cost.
Improved Compliance: The ease and accessibility of mail-in testing coupled with Fellow’s patient follow-up system can significantly improve compliance rates. Clinics using Fellow have been able to routinely achieve over 90% PVSA compliance.
Benefits for Patients:
Convenience: Mail-in testing eliminates the need for patients to take time out of their day to visit a lab. With Fellow, patients can test at a time that’s convenient for them, and avoid having to take time off work to visit a lab.
Privacy and Comfort: In person laboratory semen analysis can be an uncomfortable and embarrassing process for some patients. Mail-in testing provides a discreet option that respects patients' privacy while ensuring accurate results.
As demonstrated in the highlighted studies, compliance with post-vasectomy semen analysis has been a challenge due to various factors, including discomfort, inconvenience, and time constraints. However, the introduction of Fellow’s Vasectomy Test offers improved compliance rates by addressing the barriers of traditional PVSA methods and providing a convenient and comfortable mail-in testing process along with a convenient physician portal to track success.
Want to try Fellow at your clinic? Get in touch with the Fellow team
References:
[1] Bradshaw et al. Poor Compliance With Post vasectomy Semen Testing: Analysis of Factors and Barriers. The Journal of Urology, 2019.
[2] Duplisea et al. Understanding the factors that influence compliance with post-vasectomy semen analysis. The Journal of Urology, 2013.
[3] Trussler et al. Post-vasectomy semen analysis compliance with use of a home-based test. The Canadian Journal of Urology, 2020.
[4] Jacobson et al. Scheduling Appointments for Post vasectomy Semen Analysis Has No Impact on Compliance. European Urology Open Science, 2020.
Chief Medical Officer, Fellow